In a world increasingly preoccupied with health and wellness, the complexities of managing diabetes have spurred both scientific inquiry and individual exploration. Among the myriad approaches gaining traction, intermittent fasting has emerged as a promising strategy, captivating the attention of researchers and health enthusiasts alike. But what exactly does this eating pattern entail, and how might it intersect with the labyrinth of insulin resistance? As diabetes continues to challenge millions around the globe, understanding the potential benefits and mechanisms of intermittent fasting becomes crucial. In this article, we delve into the synergy between intermittent fasting and insulin resistance, investigating whether this practice could serve as a powerful ally in the management of diabetes. Join us as we unravel the science, explore personal narratives, and consider the implications of this dietary approach in the quest for better health.
Exploring the Connection Between Intermittent Fasting and Insulin Sensitivity
Intermittent fasting (IF) has gained popularity not just for its potential weight loss benefits but also for its impact on metabolic health, particularly insulin sensitivity. When the body undergoes periods of fasting, it shifts from glucose-based energy to fat utilization, promoting a more effective use of insulin. This process can lead to lower levels of insulin circulating in the bloodstream, which is crucial for individuals managing diabetes or seeking to improve their metabolic profile. Studies indicate that such fasting protocols can enhance insulin sensitivity, making it easier for cells to respond to insulin and uptake glucose efficiently.
Here are some key points on how intermittent fasting may positively influence insulin sensitivity:
- Reduction in Insulin Levels: Fasting lowers insulin levels, which facilitates fat burning and better glucose metabolism.
- Cellular Repair Mechanisms: IF promotes autophagy, a cellular repair process that can improve insulin receptor function.
- Enhanced Metabolic Flexibility: Fasting trains the body to switch between fuel sources, improving overall metabolic health.
The relationship between intermittent fasting and insulin sensitivity highlights its potential as a valuable tool for diabetes management. Regularly practicing IF may lead to sustained improvements in blood sugar levels and overall metabolic health. This cyclical approach to eating offers a feasible way for people to take charge of their health without complicated meal plans or strict dietary restrictions.
Unpacking the Mechanisms: How Fasting Influences Blood Sugar Levels
Fasting triggers several physiological responses in the body, which collectively contribute to more stable blood sugar levels. During periods without food intake, insulin levels decrease, allowing the body to utilize stored glycogen in the liver for energy. In this state, fat oxidation increases, and the body becomes more adept at utilizing fatty acids as an energy source. This shift not only helps in reducing excess fat but also enhances insulin sensitivity. With enhanced sensitivity, glucose uptake by the cells improves, which is especially beneficial for individuals managing blood sugar levels. It’s important to recognize that these effects are not merely anecdotal; studies have shown significant improvements in markers of blood sugar regulation following regular fasting periods.
Moreover, the impact of fasting on blood sugar levels can be visualized through the following table, highlighting key processes and their effects:
| Mechanism | Effect on Blood Sugar |
|---|---|
| Decreased Insulin Levels | Enhances glycogen breakdown and fat oxidation |
| Improved Insulin Sensitivity | Facilitates better glucose uptake in cells |
| Hormonal Changes | Promotes balance of glucagon and cortisol |
| Reduced Oxidative Stress | Improves overall metabolic function |
These adaptations not only contribute to better glycemic control but also create a more favorable metabolic environment. By alternating between feeding and fasting periods, individuals may find themselves better equipped to manage the complexities of insulin resistance and maintain healthier blood sugar patterns over time.
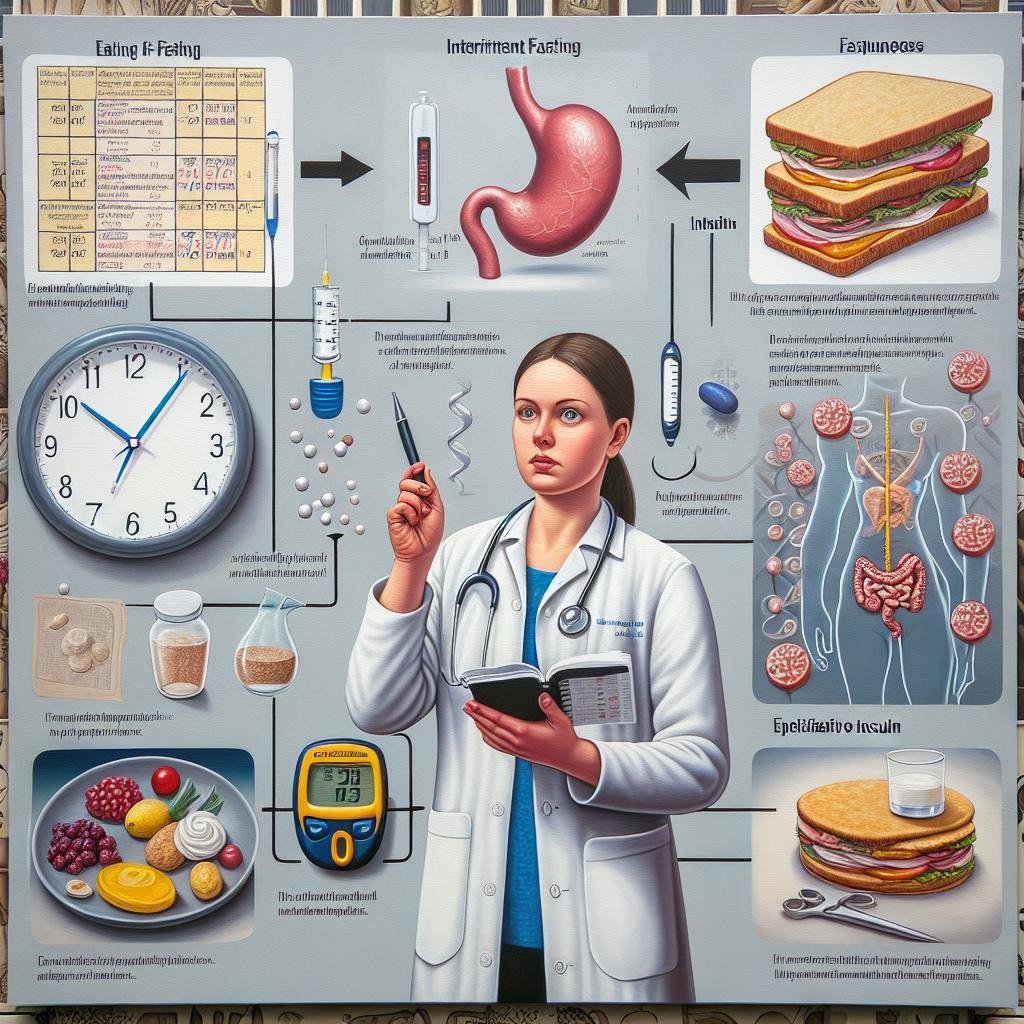
Practical Tips for Implementing Intermittent Fasting in Diabetic Management
Implementing intermittent fasting requires careful planning, especially for those managing diabetes. Begin by selecting a fasting schedule that suits your lifestyle while considering your blood sugar levels. A common approach is the 16/8 method, which involves fasting for 16 hours and eating during an 8-hour window. Prioritize nutrient-dense foods during your eating periods, focusing on whole grains, healthy fats, lean proteins, and plenty of vegetables. Maintaining adequate hydration is crucial, so drink plenty of water throughout the fasting period. Keep a log of your blood sugar levels to monitor how your body responds to fasting and adjust your plan accordingly.
To facilitate the transition to intermittent fasting, start gradually. Consider beginning with shorter fasting periods, such as 12 hours, and increasing the duration as you become comfortable. Engaging with a healthcare professional can provide personalized guidance tailored to your needs. It’s also advisable to have healthy snacks ready to prevent dips in blood sugar during your eating windows. Create a simple meal planning table to streamline your meals and ensure you’re incorporating a balance of macronutrients, such as:
| Meal | Protein Source | Healthy Fat | Fiber |
|---|---|---|---|
| Breakfast | Scrambled eggs | Avocado | Spinach |
| Lunch | Grilled chicken | Olive oil dressing | Quinoa |
| Dinner | Baked salmon | Nuts | Broccoli |

Success Stories: Real-Life Experiences of Fasting and Diabetes Control
The Conclusion
the interplay between intermittent fasting and insulin resistance presents a fascinating avenue for those looking to manage diabetes. While research indicates potential benefits—ranging from improved insulin sensitivity to weight management—individual responses can vary widely. It’s essential to approach this dietary strategy with caution, considering personal health circumstances and consulting with healthcare professionals. The journey toward better blood sugar control is often a multifaceted one, combining dietary choices, physical activity, and lifestyle adjustments. As we continue to explore the nuances of intermittent fasting, it becomes clear that knowledge and personalization are key components in navigating the complexities of diabetes. Whether you choose to embrace this eating pattern or seek alternative methods, understanding your own body’s signals will ultimately guide you toward a healthier future.