In a world increasingly captivated by the promise of health and longevity, intermittent fasting has emerged as a compelling approach to nutrition and lifestyle. As science evolves, so too does our understanding of how our bodies respond to the rhythms of eating and fasting. One of the most intriguing areas of research focuses on insulin resistance, a condition that plays a pivotal role in the development of type 2 diabetes and various metabolic disorders. Could the simple act of abstaining from food for certain periods offer a pathway to improved insulin sensitivity? This article embarks on a journey through the nuances of intermittent fasting, examining the emerging evidence and exploring the potential it holds for enhancing metabolic health. Join us as we unravel the connection between fasting and insulin resistance, shedding light on a topic that may redefine our understanding of nutrition and well-being.
Understanding Insulin Resistance and Its Implications for Health
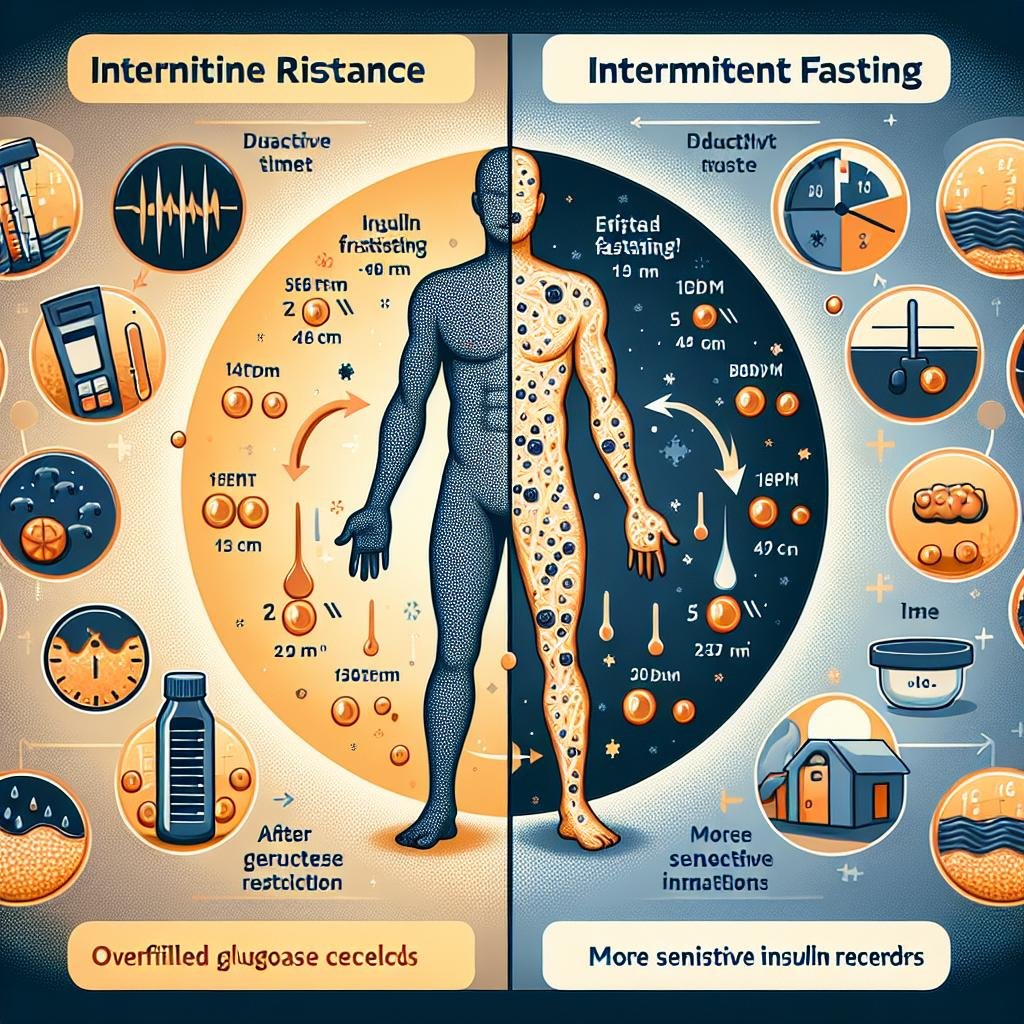
Insulin resistance is a condition where the body’s cells become less responsive to insulin, a hormone crucial for regulating blood sugar levels. This diminished response can lead to elevated blood sugar levels and increase the risk of developing type 2 diabetes, heart disease, and other metabolic disorders. Various factors, including genetics, lifestyle, and dietary habits, contribute to the onset of insulin resistance. Understanding these factors is critical as they set the stage for implementing effective strategies such as dietary adjustments and exercise routines. For many individuals, monitoring and improving insulin sensitivity becomes a pivotal aspect of maintaining overall health and preventing chronic diseases.
Recent studies have suggested that intermittent fasting may serve as a dynamic approach to countering insulin resistance. By cycling between periods of eating and fasting, individuals can influence their metabolic processes in beneficial ways. Potential benefits of this practice include:
- Enhanced cellular repair: Fasting triggers autophagy, a process that helps clear out damaged cells, potentially improving overall cellular function.
- Weight loss: Reducing caloric intake during fasting periods can aid in weight management, which is crucial for improving insulin sensitivity.
- Decrease in inflammation: Lower levels of inflammation associated with fasting may contribute to better insulin action.
To further explore how intermittent fasting affects insulin sensitivity, consider the following comparison of fasting protocols:
| Fasting Protocol | Duration | Potential Benefits |
|---|---|---|
| 16/8 Method | 16 hours fasting, 8 hours eating | Improved glucose regulation |
| 5:2 Diet | Normal eating for 5 days, reduced calories for 2 days | Weight loss and decreased insulin levels |
| Alternate-Day Fasting | 24 hours of fasting, followed by 24 hours of eating | Enhanced fat burning |
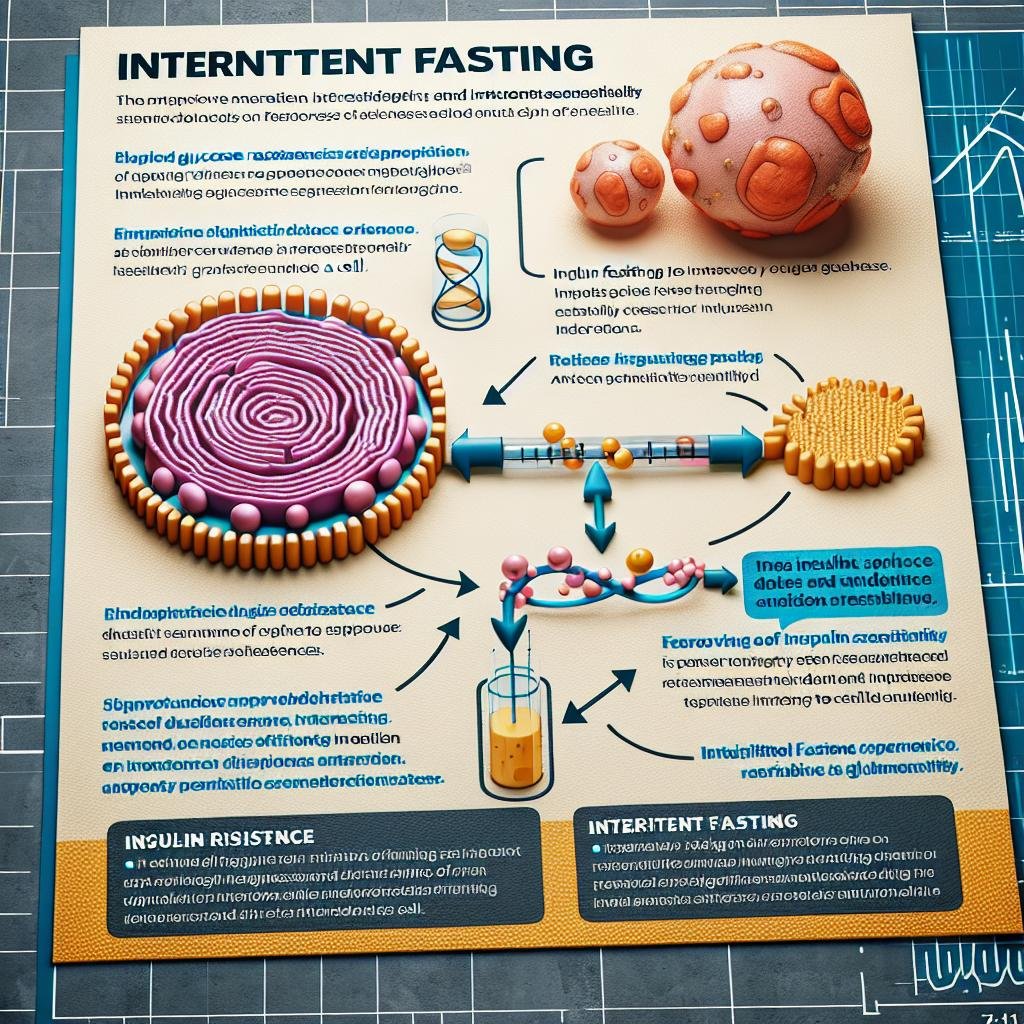
Exploring the Mechanisms of Intermittent Fasting and Its Effects on Insulin Sensitivity
Intermittent fasting (IF), a dietary pattern that cycles between periods of eating and fasting, has garnered attention for its potential to enhance metabolic health, particularly through the modulation of insulin sensitivity. During fasting periods, insulin levels drop significantly, facilitating increased fatty acid oxidation and mobilization of stored fat for energy. This reduction in insulin not only aids in weight management but also can lead to improved insulin receptor sensitivity, offering a protective factor against insulin resistance. Research suggests that the fluctuation in insulin levels during IF can lead to adaptations in the body’s ability to utilize glucose more effectively, a key factor in metabolic syndrome and type 2 diabetes prevention.
The mechanisms underlying these beneficial effects involve multiple biochemical pathways. For instance, increased autophagy during fasting can help clear damaged cells and promote cellular repair, while hormonal changes such as elevated norepinephrine enhance fat breakdown. Additionally, studies indicate that IF may modulate inflammatory pathways, thereby reducing chronic inflammation associated with insulin resistance. A summary of these mechanisms can be encapsulated as follows:
| Mechanism | Effect |
|---|---|
| Reduced Insulin Levels | Enhances fat oxidation and improves glucose uptake. |
| Increased Autophagy | Promotes cellular repair and reduces damage. |
| Hormonal Changes | Aids in fat breakdown and energy mobilization. |
| Reduced Inflammation | Decreases disease risk related to insulin resistance. |
Practical Approaches to Implementing Intermittent Fasting
Implementing intermittent fasting can be an accessible and effective strategy for improving insulin sensitivity. One practical approach is to start with a 16/8 fasting method, which involves fasting for 16 hours and eating within an 8-hour window. This method can seamlessly integrate into your lifestyle by allowing you to skip breakfast and limit your eating to lunch and dinner. Keep your meals nutrient-dense, focusing on whole foods like vegetables, lean proteins, and healthy fats. Tracking your food intake can help ensure that you’re getting enough nutrition while providing insight into how your body responds to fasting.
Another effective strategy is to experiment with alternate-day fasting or 5:2 fasting, where you eat normally for five days and restrict calories on two non-consecutive days. This variation can lessen the monotony of fasting and may suit those who find daily restrictions challenging. During fasting days, focus on hydration, consuming water, herbal teas, or black coffee to help curb hunger. Additionally, consider incorporating light physical activity, such as walking or yoga, which can enhance insulin sensitivity and improve overall well-being.
Long-Term Benefits of Fasting for Managing Insulin Resistance
Embracing fasting as a regular practice can lead to significant long-term improvements in insulin sensitivity, which may offer a pathway for individuals battling insulin resistance. When the body undergoes periods of fasting, it shifts from using glucose as its primary energy source to utilizing fat stores, a transition that is instrumental in improving metabolic health. The reduction in overall caloric intake that often accompanies fasting can contribute to sustained weight loss, which is a critical factor in enhancing insulin function. Benefits include:
- Reduced inflammation – Fasting has been shown to lower markers of inflammation, which is beneficial for those with insulin resistance.
- Improved fat oxidation – Enhanced fat-burning capabilities can lead to better blood sugar control.
- Hormonal balance – Fasting influences insulin and glucagon levels, promoting a more favorable hormonal environment.
Moreover, the metabolic flexibility gained from intermittent fasting helps the body adapt more efficiently to dietary changes. Studies have indicated that consistent fasting can lead to lower fasting insulin levels and improved glucose tolerance over time. To quantify these benefits, consider the following table illustrating common metrics observed in individuals practicing intermittent fasting:
| Metric | Before Fasting | After 3 Months of Fasting |
|---|---|---|
| Fasting Insulin (µU/mL) | 12 | 7 |
| HOMA-IR Index | 3.5 | 1.8 |
| Weight Loss (lbs) | 0 | -10 |
integrating fasting into one’s lifestyle can cultivate a resilient metabolic state conducive to improved insulin sensitivity, making it a promising strategy for individuals looking to manage insulin resistance effectively.
The Way Forward
the intricate dance between intermittent fasting and insulin resistance presents a fascinating landscape for both researchers and those grappling with metabolic health challenges. While the current evidence suggests that embracing periods of fasting might foster improved insulin sensitivity for many, it’s essential to remember that individual responses can vary widely. As we continue to unravel the complexities of our bodies and their responses to dietary patterns, intermittent fasting stands out as a potential ally in the journey toward better metabolic health.
As you explore this strategy, consider your personal lifestyle, preferences, and health goals. Consulting with healthcare professionals can further guide you on this path. Whether you’re drawn to intermittent fasting for its potential health benefits or simply out of curiosity, your journey could pave the way for a deeper understanding of how our food choices shape not just our lives but also our overall well-being. Embrace the knowledge, listen to your body, and step forward into the future of health with confidence.